As parents, it’s not unusual for sex not to be a top priority. Babies and kids need a lot of attention, and it can be hard to find the time and energy to connect with your partner.
Everyone defines a satisfactory — even great — sex life a little differently. But what’s true for anyone is that certain signs indicate you should focus on your sexual health.
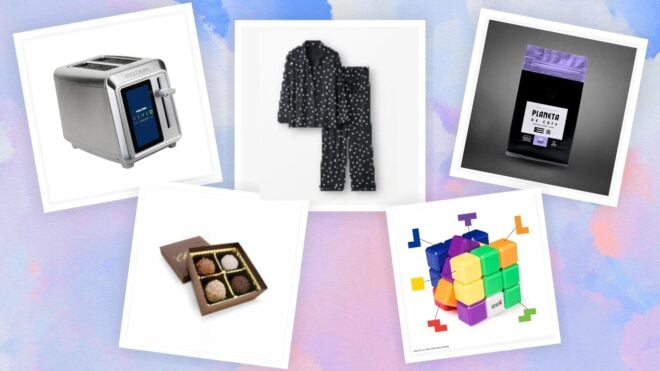
More from Mom.com: 14 Gifts for New Moms to Help Them Get the Rest They Need
There's Pain During Sex

If you experience sudden pain during sex, first let your partner know you need to stop or change positions. Recurring pain could be a sign of something more serious, such as ovarian cysts, endometriosis, or a sexually transmitted infection. Take it seriously, and seek help from your doctor.
There's Pain After Sex

Pain in the minutes or hours after sex could also indicate health issues such as a disease, an infection like thrush or an STI, menopause, a physical problem, or even psychological issues. Pain is a sign that something isn’t right. Focus on finding the source and treating it.
No Desire

Waxing and waning desire is normal, particularly if you’re in a long-term relationship. But if your lack of desire is persistent, making you unhappy, or causing you concern, it’s important to talk to your doctor. It could be a sign of changing hormones, depression, or relationship issues. Don’t assume it will fix itself.
You're Never Aroused

The inability to get aroused can be a sign of erectile dysfunction. In a 2010 study of 800 men, those who reported fewer sexual thoughts and desires were more likely nine years later to suffer from ED. Women can suffer from lack of arousal, too, often a side effect of medications, menopause, relationship issues, or depression.
You Can't Orgasm

Anorgasmia, the inability to orgasm, has several causes, such as sexual inhibition, inexperience, guilt, past sexual trauma, and other mental health reasons. It can also be caused by certain medications, chronic diseases, or simply insufficient stimulation. Orgasm is one of the great pleasures in life, and if you are missing this aspect, your doctor might be able to help.
It's Been Awhile

If it’s been a while, but you’re going back in, understand that your vagina might be drier, it may take longer to get aroused than in the past, and former favorite positions might no longer work for you. But don’t give up! Focus on what your body — and mind — need. Work with your partner to ease back in.
Vaginal Dryness

Aging, changing hormones, and certain medications might cause vaginal dryness. Many over-the-counter products will give you what you need. If you’re worried that dryness is excessive, or you think it’s contributing to pain during sex and products haven’t helped, reach out to your doctor for ideas and possible prescriptions.
You Suffer Incontinence

Urinary incontinence is bad enough, but a recent study found that it might be connected to sexual health problems, including lowered desire and lack of arousal. The good news is, incontinence is often easily treatable. Don’t be embarrassed to share what’s going on with your doctor.
Something Feels Different

Bodies change over time, and that can change how sex feels to us and our partners. If the change in feeling is unpleasant or painful, it’s important to talk about it with your partner and your doctor. Sex should be pleasurable. Neither partner should tolerate even minor discomforts.
You Had Unsafe Sex

If you recently had unsafe sex, for your own health and that of your partners, you should do more than simply regret it. Make an appointment to get tested for sexually transmitted infections. Take a pregnancy test, if it’s possible you are pregnant. Look into how things went wrong and why you had unprotected sex. Run through scenarios for how to avoid unprotected sex in the future.
You Have an STI

If you were diagnosed with an STI, such as gonorrhea, chlamydia, herpes simplex virus, or something else, understand how you got it, contact subsequent partners, and follow your treatment protocols. If you’re exhibiting symptoms of STIs, such as itching, sores, or a burning sensation when you pee, don’t assume it’s a UTI or yeast infection. Get tested and treated.
You Have Multiple Partners

Non-exclusive sexual relationships come with risks to one’s health, especially greater exposure to STIs. Prioritizing health in any sexual relationship lowers your risk. No sex is 100 percent safe, so it should be met with protections both from disease and, if applicable, pregnancy.
You're Having an Affair

Likewise, if you’re having an affair, you need to take precautions with each encounter, not only for your health but also for your partner at home. The Centers for Disease Control and Prevention recommends getting tested annually (or more often) for STIs, depending on your risk categories. Disclose to your partners if you test positive — which might be difficult but is definitely necessary.
You're Depressed

Often depression can cause sexual dysfunction, such as low to no libido, diminished arousal, or inability to orgasm. Likewise, sometimes sexual dysfunction or issues can lead to depression. Let your therapist or doctor know about both and understand your treatment options.
Mismatched Sex Drives

Mismatched sex drives can be corrosive in a relationship. It can lead to frustration and feelings of rejection for the partner desiring more sex while distancing the other partner who can’t bring it as often. Each partner owes it to their own sexual health to talk about it with professionals and find ways to make it work.
You're Having Chemo

Chemo can, among other things, complicate sex lives. It can change hormone levels, leave you too tired for sex, or make you self-conscious about your body. Sometimes chemo makes having an orgasm difficult or impossible. If you enjoyed sex before chemo, don’t give up on sex altogether. Talk to your doctor about how you’re feeling. Ask for referrals for therapy, pharmaceuticals, or reconstruction.
Unusual Bleeding

Bleeding after sex, even if you experience it regularly, should not be ignored. It can be the consequence of something more serious, such as an infection or pelvic disorders. Or it could mean you’re suffering from vaginal dryness, for which there are many over-the-counter solutions. You might also have hormone issues, which can also be treated by your doctor.
Unusual Discharge

Pay attention to unusual discharge, which can be a side effect of antibiotics, birth control pills, or menopause. It can also indicate more serious health issues such as an STI, pelvic inflammatory disease, yeast infections, diabetes, or even cervical cancer. Talk to your doctor about what you’re noticing, making notes of amount, consistency, color, and odor.
Recurring UTI

Urinary tract infections are the most frequent bacterial infection in women. They’re often caused by improper wiping — the safest way is front to back — complacent hygiene or sex. Staying hydrated and making sure you pee after sex is one of the most consistent ways to lower your risk for UTIs. In any case, let your doctor know so you can rule out more serious issues — and prevent serious cases of infection to the kidneys.
Frequent Yeast Infections

Vaginal yeast infections are now easily treatable with over-the-counter options. But if you’re getting frequent yeast infections, you should talk to your doctor to rule out more serious issues, such as diabetes, a weakened immune system, or too-strong birth control pills. Yeast infections are not considered STIs, but you can get one from your partner. Using condoms and dental dams can prevent transmission.